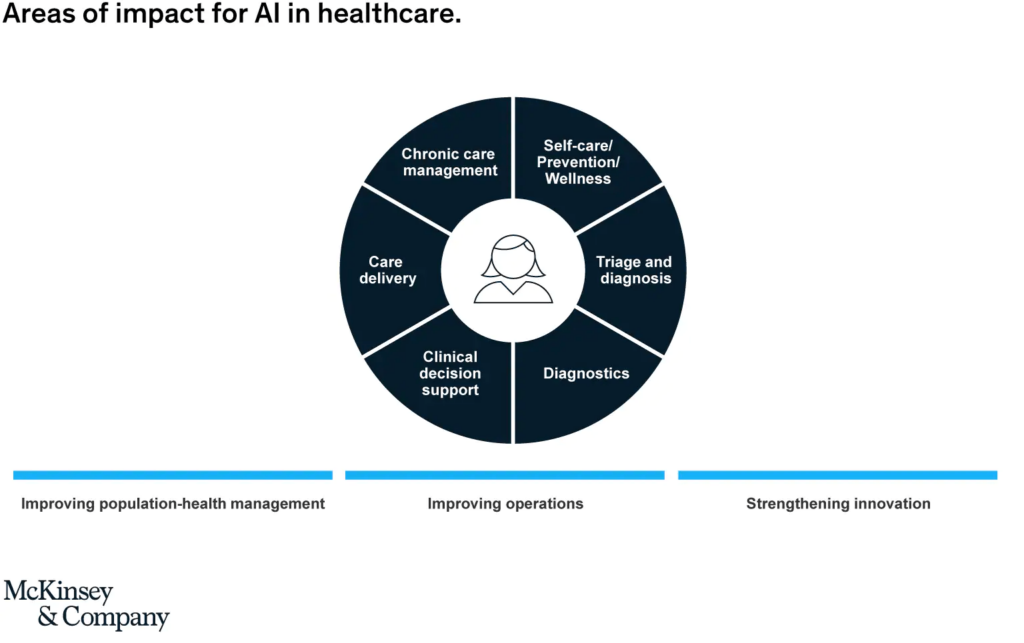
What do we mean by Artificial intelligence (AI) in healthcare? In this report we include applications that affect care delivery, including both how existing tasks are performed and how they are disrupted by changing healthcare needs or the processes required to address them, says McKinsey.
We also include applications that enhance and improve healthcare delivery, from day-to-day operational improvement in healthcare organizations to population-health management and the world of healthcare innovation.
AI is Modernizing the HealthCare
It’s a broad definition that covers natural language processing (NLP), image analysis, and predictive analytics based on machine learning.
As such, it illustrates a spectrum of AI solutions, where encoding clinical guidelines or existing clinical protocols through a rules-based system often provides a starting point, which then can be augmented by models that learn from data.
AI is now top-of-mind for healthcare decision makers, governments, investors and innovators, and the European Union itself. An increasing number of governments have set out aspirations for AI in healthcare, in countries as diverse as Finland, Germany, the United Kingdom, Israel, China, and the United States and many are investing heavily in AI-related research.
The private sector continues to play a significant role, with venture capital funding for the top 50 firms in healthcare-related AI reaching $8.5 billion, and big tech firms, startups, pharmaceutical and medical-devices firms and health insurers, all engaging with the nascent AI healthcare ecosystem.
Geographically, the dynamics of AI growth are shifting. The United States still dominates the list of firms with highest VC funding in healthcare AI to date, and has the most completed AI-related healthcare research studies and trials.
But the fastest growth is emerging in Asia, especially China, where leading domestic conglomerates and tech players have consumer-focused healthcare AI offerings.
Europe, meanwhile, benefits from the vast troves of health data collected in national health systems and has significant strengths in terms of the number of research studies, established clusters of innovation and pan-European collaborations, a pan-European approach to core aspects of AI (e.g., ethics, privacy, “trustworthy AI”) and an emerging strategy on how to ensure the “EU way” for AI helps deliver the advantages for AI to its population. Yet, at the same time, valuable data sets are not linked, with critical data-governance, access, and security issues still needing to be clarified, delaying further adoption.
European investment and research in AI are strong when grouped together but fragmented at the country or regional level. Overall, there is a significant opportunity for EU health systems, but AI’s full potential remains to be explored and the impact on the ground remains limited.
A surprising 44% of the healthcare professionals we surveyed—and these were professionals chosen based on their engagement with healthcare innovation—had never been involved in the development or deployment of an AI solution in their organization.
Growing number of use cases
While there are widespread questions on what is real in AI in healthcare today, this report looked at 23 applications in use today and provides case studies of 14 applications already in use. These illustrate the full range of areas where AI can have impact: from apps that help patients manage their care themselves, to online symptom checkers and e-triage AI tools, to virtual agents that can carry out tasks in hospitals, to a bionic pancreas to help patients with diabetes. Some help improve healthcare operations by optimizing scheduling or bed management, others improve population health by predicting the risk of hospital admission or helping detect specific cancers early enabling intervention that can lead to better survival rates; and others even help optimize healthcare R&D and pharmacovigilance. The scale of many solutions remains small, but their increasing adoption at the health-system level indicates the pace of change is accelerating. In most cases, the question is less whether AI can have impact, and more how to increase the potential for impact and, crucially, how to do so while improving the user experience and increasing user adoption.
Three phases of scaling AI in healthcare
We are in the very early days of our understanding of AI and its full potential in healthcare, in particular with regards to the impact of AI on personalization. Nevertheless, interviewees and survey respondents conclude that over time we could expect to see three phases of scaling AI in healthcare, looking at solutions already available and the pipeline of ideas.
First, solutions are likely to address the low-hanging fruit of routine, repetitive and largely administrative tasks, which absorb significant time of doctors and nurses, optimizing healthcare operations and increasing adoption. In this first phase, we would also include AI applications based on imaging, which are already in use in specialties such as radiology, pathology, and ophthalmology.
In the second phase, we expect more AI solutions that support the shift from hospital-based to home-based care, such as remote monitoring, AI-powered alerting systems, or virtual assistants, as patients take increasing ownership of their care. This phase could also include a broader use of NLP solutions in the hospital and home setting, and more use of AI in a broader number of specialties, such as oncology, cardiology, or neurology, where advances are already being made.
This will require AI to be embedded more extensively in clinical workflows, through the intensive engagement of professional bodies and providers. It will also require well designed and integrated solutions to use existing technologies effectively in new contexts. This scaling up of AI deployment would be fuelled by a combination of technological advancements (e.g., in deep learning, NLP, connectivity etc.) and cultural change and capability building within organizations.
In the third phase, we would expect to see more AI solutions in clinical practice based on evidence from clinical trials, with increasing focus on improved and scaled clinical decision-support (CDS) tools in a sector that has learned lessons from earlier attempts to introduce such tools into clinical practice and has adapted its mind-set, culture and skills.
Ultimately respondents would expect to see AI as an integral part of the healthcare value chain, from how we learn, to how we investigate and deliver care, to how we improve the health of populations. Important preconditions for AI to deliver its full potential in European healthcare will be the integration of broader data sets across organizations, strong governance to continuously improve data quality, and greater confidence from organizations, practitioners and patients in both the AI solutions and the ability to manage the related risks.








