1,514,000 Medicaid enrollees have been disenrolled, based on the most current data from 25 states and the District of Columbia, according to KFF.
Overall, 37% of people with a completed renewal were disenrolled in reporting states while 63%, or 2.5 million enrollees, had their coverage renewed.
Because not all states have publicly available data on total disenrollments, the data reported here undercount the actual number of disenrollments.

There is wide variation in disenrollment rates across reporting states, ranging from 81% in South Carolina to 16% in Virginia.
Disenrolled in 25 states and DC
At least 1,514,000 Medicaid enrollees have been disenrolled in 25 states and DC with publicly available unwinding data
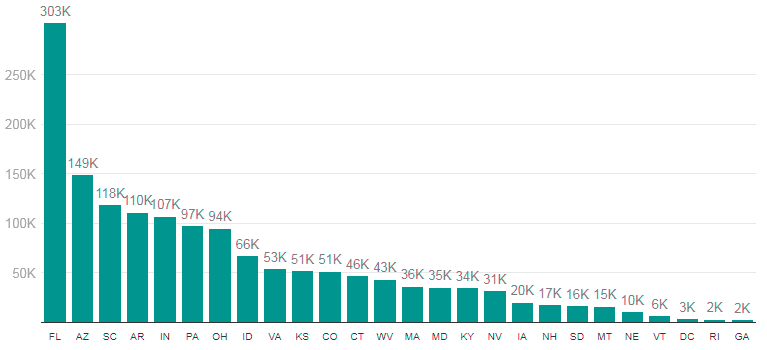
SOURCE: KFF Analysis of State Unwinding Dashboards and Monthly Reports Submitted to CMS
Disenrollment rates across reporting states
There is wide variation in disenrollment rates across reporting states, ranging from 81% in South Carolina to 16% in Virginia
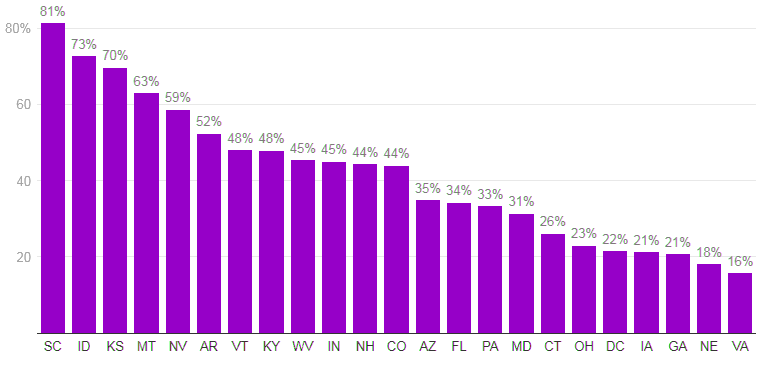
SOURCE: KFF Analysis of State Unwinding Dashboards and Monthly Reports Submitted to CMS
Differences in who states are targeting with early renewals as well as differences in renewal policies and systems capacity likely explain some of the variation in disenrollment rates.
Some states (such as South Carolina) are initially targeting people early in the unwinding period that they think are no longer eligible or who did not respond to renewal requests during the pandemic, but other states are conducting renewals based on an individual’s renewal date.
Additionally, some states have adopted several policies that promote continued coverage among those who remain eligible and have automated eligibility systems that can more easily and accurately process renewals while other states have adopted fewer of these policies and have more manually-driven systems.

Across all states with available data, 73% of all people disenrolled had their coverage terminated for procedural reasons.
There is also wide variation in rates of procedural disenrollments across states reporting this breakout, ranging from 95% in South Carolina to 28% in Iowa.
73% of disenrollments are due to procedural reasons, among states reporting
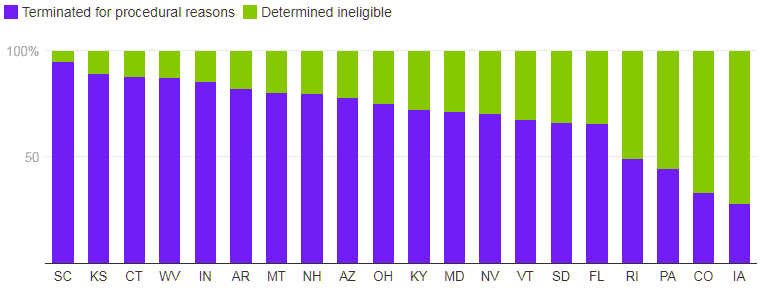
SOURCE: KFF Analysis of State Unwinding Dashboards and Monthly Reports Submitted to CMS
Procedural disenrollments are cases where people are disenrolled because they did not complete the renewal process and can occur when the state has outdated contact information or because the enrollee does not understand or otherwise does not complete renewal packets within a specific timeframe.
High procedural disenrollment rates are concerning because many people who are disenrolled for these paperwork reasons may still be eligible for Medicaid coverage.
The Medicaid continuous enrollment provision, which had halted Medicaid disenrollments since March 2020, ended on March 31, 2023.
Primarily due to the continuous enrollment provision, KFF estimates that enrollment in Medicaid/CHIP grew by 23.3 million to nearly 95 million from February 2020 to the end of March 2023.
As states unwind the continuous enrollment provision over the following 12 months, they will redetermine eligibility for all Medicaid enrollees and will disenroll those who are no longer eligible or who may remain eligible but are unable to complete the renewal process. Millions of people are expected to lose Medicaid coverage during this unwinding period.
2023 Medicaid & CHIP Enrollment Data Highlights

All states—including the District of Columbia—provide data each month about their Medicaid and Children’s Health Insurance Programs (CHIP) eligibility and enrollment activity.
93,373,794 individuals were enrolled in Medicaid and CHIP in the 50 states and the District of Columbia that reported enrollment data for February 2023.
- 86,174,094 individuals were enrolled in Medicaid.
- 7,199,700 individuals were enrolled in CHIP.
41,977,712 individuals were enrolled in CHIP or were children enrolled in the Medicaid program in the 49 states and the District of Columbia that reported child enrollment data for February 2023 representing 46% of total Medicaid and CHIP program enrollment.
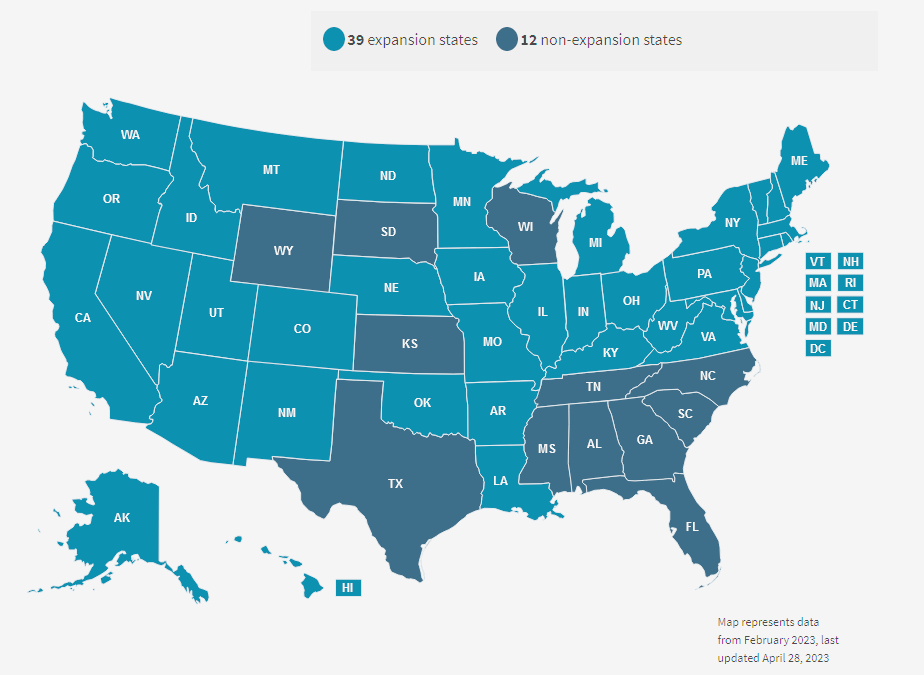
Medicaid Expansion Status
Child Enrollment (Medicaid Child + CHIP Enrollment)
Child Enrollment (Medicaid Child + CHIP Enrollment) figures represent the number of children enrolled in the Medicaid program and the total enrollment for separate CHIP programs as of the last day of the reporting period.
These figures are point-in-time counts of total program enrollment, and not solely counts of those newly enrolled during the reporting period. These figures include only those individuals who are eligible for comprehensive benefits (for example, emergency Medicaid, family planning-only coverage and limited benefit dual eligible individuals are excluded).
States use the definition of “child” as included in the state’s Medicaid or CHIP state plan in reporting performance indicator data to the Centers for Medicare & Medicaid Services (CMS), which varies from state to state.
Total Medicaid and CHIP Enrollment
Total enrollment figures represent the total unduplicated number of individuals enrolled in Medicaid and CHIP as of the last day of the reporting period. These figures are point-in-time counts of total program enrollment, and not solely a count of those newly enrolled during the reporting period.
These figures include only those individuals who are eligible for comprehensive benefits (for example, emergency Medicaid, family planning-only coverage and limited benefit dual eligible individuals are excluded), except as indicated in the state-specific notes included with the tables.
Other Sources of Enrollment Data
CMS collects Medicaid and CHIP enrollment data from states through multiple reporting vehicles, such as Statistical Enrollment Data System (SEDS) and Medicaid Budget and Expenditure System.
These enrollment data may not align with the data included in this report because of methodological differences. For example, in the most recent published SEDS annual enrollment report, CHIP enrollment was reported as more than 9.6 million.
Unlike the point-in-time, monthly enrollment counts included in this report, the SEDS CHIP enrollment figure represents the number of individuals ever enrolled in CHIP throughout the year.
What’s the difference between Medicare and Medicaid?
Medicare
Medicare is federal health insurance for people 65 or older, and some people under 65 with certain disabilities or conditions.
A federal agency called the Centers for Medicare & Medicaid Services runs Medicare. Because it’s a federal program, Medicare has set standards for costs and coverage.
This means a person’s Medicare coverage will be the same no matter what state they live in.
Medicare-related bills are paid from two trust funds held by the U.S. Treasury. Different sources (including payroll taxes and funds that Congress authorizes) fund the trust funds. People with Medicare pay part of the costs through things like monthly premiums for medical and drug coverage, deductibles and coinsurance.
For more information, visit Medicare.gov.
Medicaid
Medicaid is a joint federal and state program that helps cover medical costs for some people with limited income and resources.
The federal government has general rules that all state Medicaid programs must follow, but each state runs its own program.
This means eligibility requirements and benefits can vary from state to state.
Medicaid offers benefits that Medicare doesn’t normally cover, like nursing home care and personal care services. People with Medicaid usually don’t pay anything for covered medical expenses but may owe a small co-payment for some items or services.
For more information, visit Medicaid.gov.
…………………..
Edited by 








